Chest Percussion
Introduction
By tapping on the chest, you can detect abnormal sounds and vibrations, providing valuable insights into the patient’s lung function and any underlying pathology. Whilst percussing you can determine whether the lungs are filled with air, fluid, or solid material. Chest percussion can also be useful to evaluate the distance the diaphragm travels.
In the prehospital environment, the application of percussion may be limited due to environmental factors – however, this should not deter you from carrying out this assessment.
Areas
Percussion can assess organs as deep as 3 inches. As percussion is carried out around the chest, you’ll hear different percussion sounds in different areas of the chest.
Areas to percussion should include:
- Axilla
- Chest wall
- Infraclavicular region
- Supraclavicular region
Percussion should be carried out laterally to assess each side of the chest at each percussion point. Percussion should be performed over intercostal space. The image below shows the sequence that should be used when percussing the chest.
Technique
Correct technique when percussing is essential to generate effective notes.
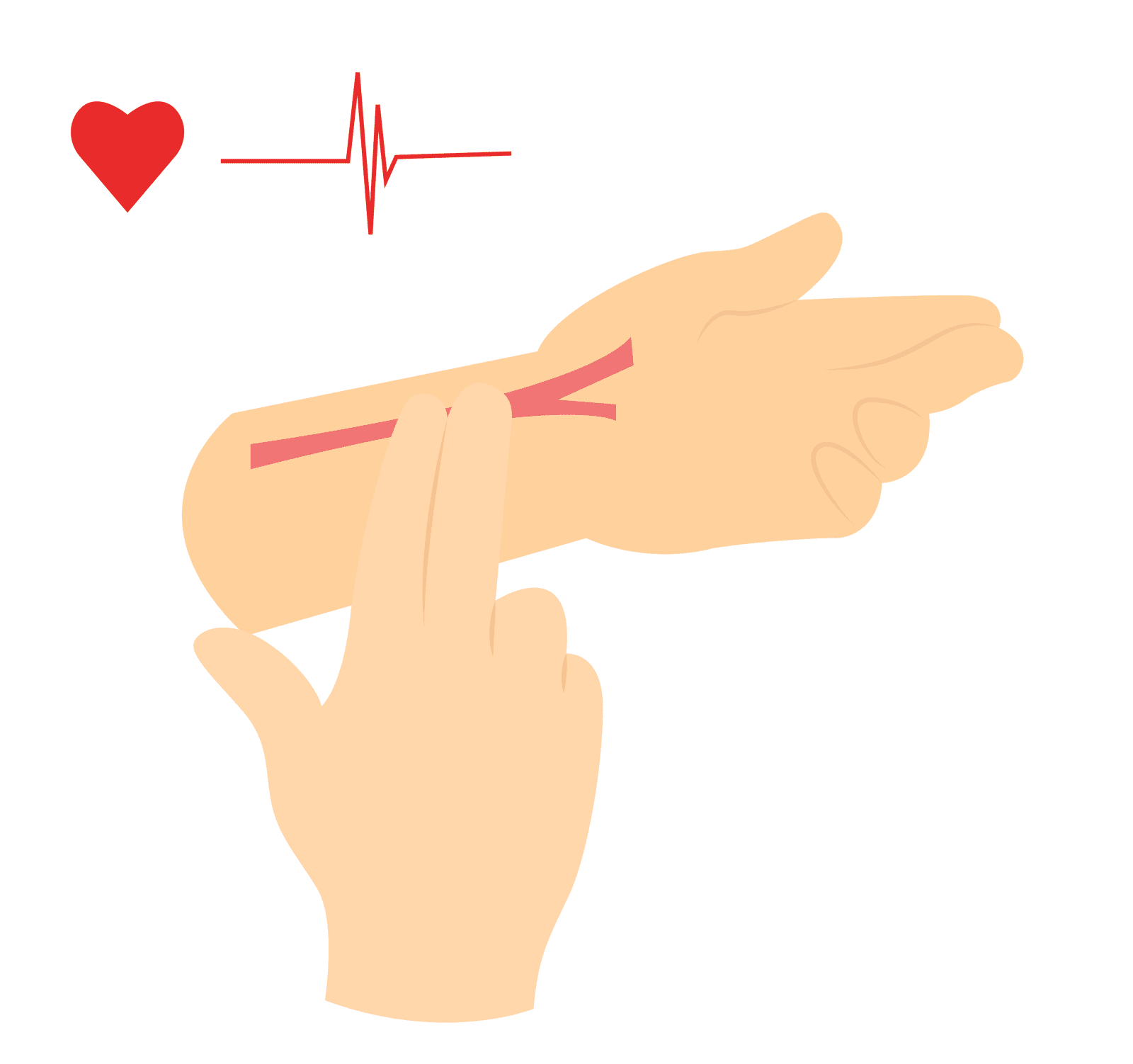
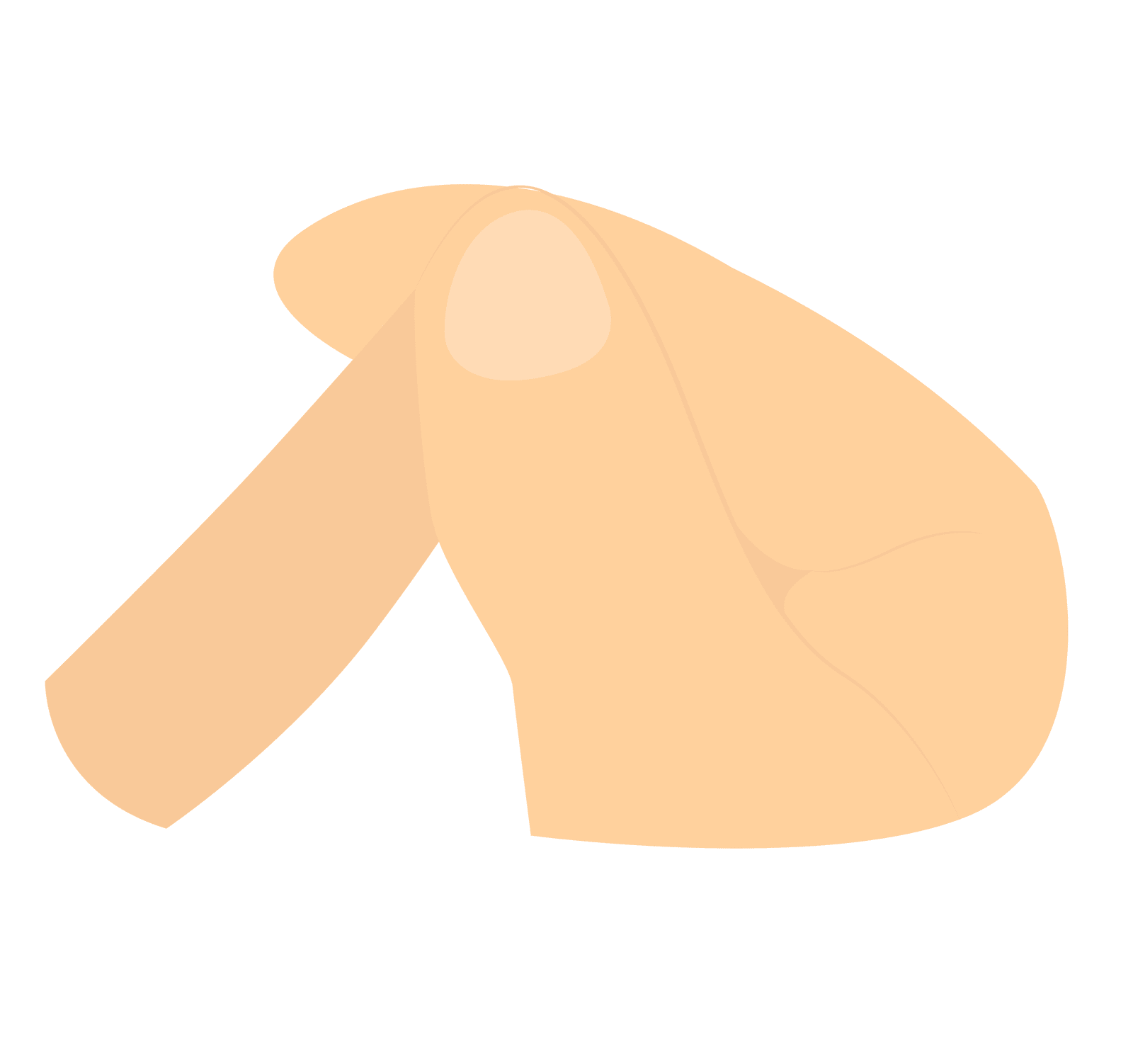
Place your non-dominant hand on the chest wall while hyperextending the middle finger and placing it over the percussion area.
With the dominant hand’s middle finger, tap the middle phalanx of the hand above. The movement should come from the wrist rather than the elbow or upper arm.
Follow the percussion sequence shown above and note any abnormal findings.
Fingernails should be kept short on the dominant tapping hand as to not hurt yourself when striking the non-dominant hand.
Findings
Resonant (Normal Sound)
This is a loud low-pitch sound that is hollow and is normally heard when percussing the lungs as they are filled with air rather than dense tissue.
However, a dull sound should be heard over organs such as the heart (located in the anterior left of the chest at the third/fourth intercostal space).
Hyperresonant
This is a very loud, lower-pitched sound and has a longer duration than resonance.
This could suggest hyperinflated lung such as bullous emphysema, pneumothorax, or acute asthma.
Tympanic
This is a loud, high-pitched sound that is similarly sounding to a drum. This is longer than both resonance and hyperresonance.
This may suggest a large pneumothorax.
Dull
This sounds thud like with a high pitch and short duration.
Dullness represents solid area such as organs or abnormal pathology in area where it should be sounding resonant suggesting lobar pneumonia, pleural fluid, tumour.
Flat
Quieter than dullness with a short, soft, high-pitched sound.
This can sound when percussing muscle or bone but may also suggest consolidation as in atelectasis or extensive pleural effusion.
Diaphragm Measurement
Percussion also enables you to assess diaphragm movement. Normal diaphragm movement ranges between 3-5cm.
Ask the patient to exhale, once fully exhaled percuss the back on one side to locate the upper edge of the diaphragm (noticeable change from resonance to dullness). Make this spot. Repeat this on the other side of the back.
Repeat the above process when the patient has inhaled fully.
Measure the distance between the two marks with normal range between 3-5cm. The distance should also be the same on both sides of the back.
Decreased diaphragm movement may suggest emphysema, respiratory depression, paralysis, obesity, ascites, or atelectasis.
Key Points
- Chest percussion can help in diagnosing various respiratory conditions, including pneumonia, pleural effusion, emphysema, and pneumothorax.
- When performing chest percussion, it is essential to compare the sounds and vibrations on the left side of the chest with the right side and vice versa.
- Resonance is the normal, hollow sound heard over healthy lung tissue. Remember to think about the anatomy and take into consideration when hearing different sounds (e.g., dullness over the heart)
Bibliography
Blaber, A. and Harris, G. (2021). Assessment skills for paramedics. 3rd ed. Maidenhead, England: Open Univ Press.
Williams, L. (2013). Assessment made incredibly easy! Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.
Introduction
By tapping on the chest, you can detect abnormal sounds and vibrations, providing valuable insights into the patient’s lung function and any underlying pathology. Whilst percussing you can determine whether the lungs are filled with air, fluid, or solid material. Chest percussion can also be useful to evaluate the distance the diaphragm travels.
In the prehospital environment, the application of percussion may be limited due to environmental factors – however, this should not deter you from carrying out this assessment.
Areas
Percussion can assess organs as deep as 3 inches. As percussion is carried out around the chest, you’ll hear different percussion sounds in different areas of the chest.
Areas to percussion should include:
- Axilla
- Chest wall
- Infraclavicular region
- Supraclavicular region
Percussion should be carried out laterally to assess each side of the chest at each percussion point. Percussion should be performed over intercostal space. The image below shows the sequence that should be used when percussing the chest.
Technique
Correct technique when percussing is essential to generate effective notes.
Place your non-dominant hand on the chest wall while hyperextending the middle finger and placing it over the percussion area.
With the dominant hand’s middle finger, tap the middle phalanx of the hand above. The movement should come from the wrist rather than the elbow or upper arm.
Follow the percussion sequence shown above and note any abnormal findings.
Fingernails should be kept short on the dominant tapping hand as to not hurt yourself when striking the non-dominant hand.
Findings
Resonant (Normal Sound)
This is a loud low-pitch sound that is hollow and is normally heard when percussing the lungs as they are filled with air rather than dense tissue.
However, a dull sound should be heard over organs such as the heart (located in the anterior left of the chest at the third/fourth intercostal space).
Hyperresonant
This is a very loud, lower-pitched sound and has a longer duration than resonance.
This could suggest hyperinflated lung such as bullous emphysema, pneumothorax, or acute asthma.
Tympanic
This is a loud, high-pitched sound that is similarly sounding to a drum. This is longer than both resonance and hyperresonance.
This may suggest a large pneumothorax.
Dull
This sounds thud like with a high pitch and short duration.
Dullness represents solid area such as organs or abnormal pathology in area where it should be sounding resonant suggesting lobar pneumonia, pleural fluid, tumour.
Flat
Quieter than dullness with a short, soft, high-pitched sound.
This can sound when percussing muscle or bone but may also suggest consolidation as in atelectasis or extensive pleural effusion.
Diaphragm Measurement
Percussion also enables you to assess diaphragm movement. Normal diaphragm movement ranges between 3-5cm.
Ask the patient to exhale, once fully exhaled percuss the back on one side to locate the upper edge of the diaphragm (noticeable change from resonance to dullness). Make this spot. Repeat this on the other side of the back.
Repeat the above process when the patient has inhaled fully.
Measure the distance between the two marks with normal range between 3-5cm. The distance should also be the same on both sides of the back.
Decreased diaphragm movement may suggest emphysema, respiratory depression, paralysis, obesity, ascites, or atelectasis.
Key Points
- Chest percussion can help in diagnosing various respiratory conditions, including pneumonia, pleural effusion, emphysema, and pneumothorax.
- When performing chest percussion, it is essential to compare the sounds and vibrations on the left side of the chest with the right side and vice versa.
- Resonance is the normal, hollow sound heard over healthy lung tissue. Remember to think about the anatomy and take into consideration when hearing different sounds (e.g., dullness over the heart)
Bibliography
Blaber, A. and Harris, G. (2021). Assessment skills for paramedics. 3rd ed. Maidenhead, England: Open Univ Press.
Williams, L. (2013). Assessment made incredibly easy! Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.