Pulse
Introduction
Pulse serves as a key indicator of overall cardiovascular health and provides valuable information regarding heart rate, rhythm, and strength. Monitoring the pulse is a fundamental aspect of any medical assessment, allowing gathering of essential data about a person’s circulatory system. A pulse should be assessed on every patient.
A pulse is the rhythmic expansion and contraction of arteries during each cardiac cycle. It is felt when the pressure waves passes through the arterial tree. It is felt by palpating an artery (compressing the artery against firm tissue) that lies close to the surface of the skin.
There are a variety of sites that a pulse can be felt, but due to accessibility the radial pulse is most used.
Pulse Sites

Carotid Artery
Subclavian Artery
Brachial Artery
Radial Artery
Ulna Artery
Femoral Artery
Popliteal Artery
Dorsalis Pedis Artery
Indications
A pulse is useful to take in all patients as it allows the clinician to:
- Gather information on the patient’s cardiovascular health.
- Gain a baseline measurement.
- Provide reassurance in patients who may be anxious.
Contraindications
None.
Cautions
Taking a pulse is a routine and non-invasive procedure. However, it some situation taking a pulse may be more challenging or require special considerations such as:
- Severe limb trauma.
- Severe burns.
- Obvious arterial bleeding.
- Patient discomfit/distress.
Complications
Some very rare complications that may occur are:
- Allergic reactions (latex gloves, alcohol wipes).
- Patient discomfort or pain.
- Psychological distress.
Procedure
Carry out pre-proecdure checks.
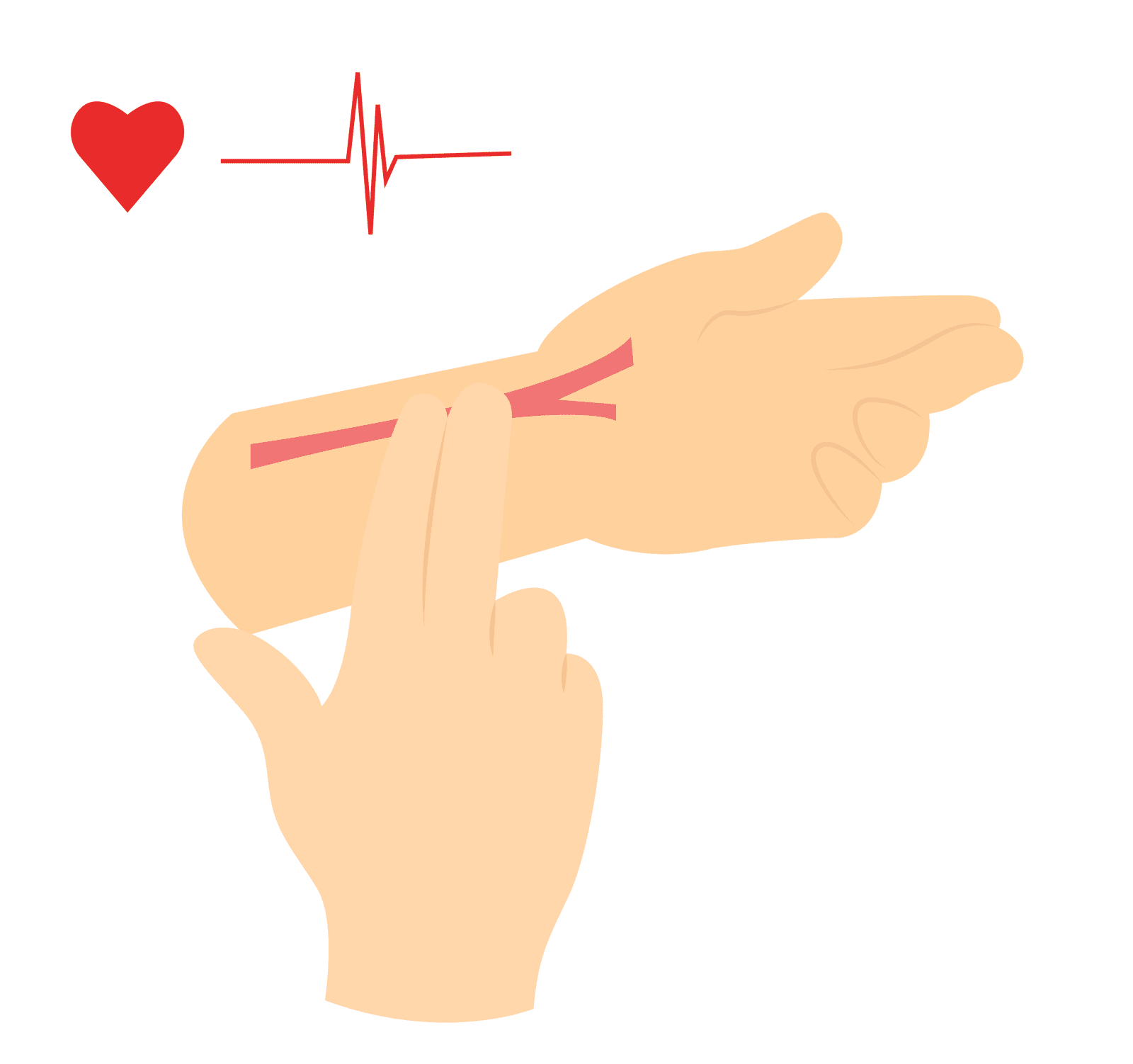
Place the first and second finger along the artery and press gently.
The thumb should not be used as it has a strong pulse which might be mistaken for the patient’s pulse. However, the thumb can be used in stronger pulses such as the brachial.
The pulse should be counted for a minimum of 15 seconds and multiplied by 4. In cases of irregular, rapid or slow beats then a 60 second count should be utilised.
Record the pulse rate on the patient record, including details about the rhythm and strength.
When taking a carotid pulse, the patient should lie down to reduce the risk of reflex bradycardia as this may cause reduction in blood pressure resulting in syncope.
Pre-Procedure Checks
Check out more information on how to carry out pre-procedure checks.
Pre-Procedure Checks
Interpreting Results
Rate
Pulse rate refers to the number of times the hear beats per minute (bpm) and is a component in assessing the patient’s cardiovascular health.
Generally, a normal adult resting heart rate is between 60-100bpm. Below 60bpm is referred to as bradycardic and above 100bpm as tachycardic. However, these values are arbitrary and should be taken in context of the clinical situation.
The pulse rate is used to calculate the cardiac output, which is the volume of blood ejected by each ventricle per minute.
Cardiac Output = Heart Rate x Stroke Volume.
Hence, from the above equation, the heart rate is a factor that affects the cardiac output.
The pulse rate in a health patient tends to be relatively constant. However, in disease state of injury to the heart, the stroke volume is affected negatively (reduced), especially in cardiac muscle disease and reduced blood volume. In this case, to maintain the cardiac output, the heart rate needs to increase.
Causes of bradycardia
- Second degree heart block
- Third degree heart block
- Medication (beta blockers, digoxin)
- Sleep
- Hypothyroidism
- Athletes
Causes of tachycardia
- Pain
- Anxiety/Excitement
- Fever
- Medication (Vasodilators)
- Exercise
- Hyperthyroidism
- Cardiac arrhythmias (AF, SVT)
Rhythm
Pulse rhythm refers to the regularity or irregularity of the intervals between heartbeats. In healthy individuals, the pulse is typically regular and consistent. This regular pattern indicates the coordinated and efficient functioning of the heart’s electrical system.
Irregular pulse rhythms can occur it patients with underlying cardiovascular conditions. The irregularity in pulse rhythm is due to loss of co-ordination of the electrical conduction system (either rapid or delayed electrical discharge).
Causes of irregular pulses
- Sinus arrhythmia
- Atrial fibrillation
- Ventricular extrasystoles
- Atrial extrasystoles
- Second degree heart block
Rhythm identification
Regular
Regular intervals between heartbeats.
Irregularly irregular
Random pattern of pulsation. Normally associated with atrial fibrillation.
Regularly irregular
Irregular beat that occurs in a regular pattern, commonly seen in second degree hart blocks and pulsus bigeminies.
Regular with ectopic
Normal heart rate interrupted by an extra beat that causes the sequence to become out making the pulse feel irregularly irregular. ECG is needed to confirm this.
Strength/Character
Pulse strength or character refers to the quality and characteristics of the force of ejection of blood from the ventricles and the elasticity of the arterial wall. Different terms can be used to describe the pulse strength – weak, thready, strong, bounding, and full.
Weak/thready pulse
This can be a sign of reduced stroke volume secondary to disease or peripheral vascular disease. Causes of weak pulse can include bleeding, shock, heart failure, or dehydration.
Strong/bounding pulse
This may be felt during the times of high cardiac output or decreased peripheral resistance. Conditions such as exercise, heat, fever, anaemia, and other certain heart conditions.
Symmetry
Pulse symmetry refers to the equality or similarity of the pulses on both sides of the body. It involves comparing the rate, rhythm, and strength of the pulse inn corresponding pulse points.
This is not often routinely required unless clinical suspicion of conditions such as acute aortic dissection or obstruction of the arterial tree.
Pulses can also be felt simultaneously on the same side, such as the radial and femoral artery, and if there is a delay, this may also indicate an underlying condition.
Follow us on Facebook
Key Points
- The pulse is the rhythmic expansion and contraction of arteries caused by the heartbeat.
- It serves as a vital sign and provides information about heart rate, rhythm, and strength.
- Monitoring the pulse is crucial in assessing cardiovascular health and guiding medical interventions.
- Normal resting pulse rate for adults typically ranges between 60 and 100 beats per minute (bpm).
- Factors like age, fitness level, activity level, and underlying health conditions can influence the pulse rate.
Bibliography
British Heart Foundation (2015). What is a normal pulse rate? [online] BHF. Available at: https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/ask-the-experts/pulse-rate#:~:text=Your%20pulse%20rate%2C%20also%20known
Gregory, P. and Mursell, I. (2010). Manual of clinical paramedic procedures. Chichester: Wiley-Blackwell.
Bibliography
British Heart Foundation (2015). What is a normal pulse rate? [online] BHF. Available at: https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/ask-the-experts/pulse-rate#:~:text=Your%20pulse%20rate%2C%20also%20known
Gregory, P. and Mursell, I. (2010). Manual of clinical paramedic procedures. Chichester: Wiley-Blackwell.
Introduction
Pulse serves as a key indicator of overall cardiovascular health and provides valuable information regarding heart rate, rhythm, and strength. Monitoring the pulse is a fundamental aspect of any medical assessment, allowing gathering of essential data about a person’s circulatory system. A pulse should be assessed on every patient.
A pulse is the rhythmic expansion and contraction of arteries during each cardiac cycle. It is felt when the pressure waves passes through the arterial tree. It is felt by palpating an artery (compressing the artery against firm tissue) that lies close to the surface of the skin.
There are a variety of sites that a pulse can be felt, but due to accessibility the radial pulse is most used.
Pulse Sites

Carotid Artery
Subclavian Artery
Brachial Artery
Radial Artery
Ulna Artery
Femoral Artery
Popliteal Artery
Dorsalis Pedis Artery
Indications
A pulse is useful to take in all patients as it allows the clinician to:
- Gather information on the patient’s cardiovascular health.
- Gain a baseline measurement.
- Provide reassurance in patients who may be anxious.
Contraindications
None.Cautions
Taking a pulse is a routine and non-invasive procedure. However, it some situation taking a pulse may be more challenging or require special considerations such as:
- Severe limb trauma.
- Severe burns.
- Obvious arterial bleeding.
- Patient discomfit/distress.
Complications
Some very rare complications that may occur are:
- Allergic reactions (latex gloves, alcohol wipes).
- Patient discomfort or pain.
- Psychological distress.
Procedure
Carry out pre-proecdure checks.
Place the first and second finger along the artery and press gently.
The thumb should not be used as it has a strong pulse which might be mistaken for the patient’s pulse. However, the thumb can be used in stronger pulses such as the brachial.
The pulse should be counted for a minimum of 15 seconds and multiplied by 4. In cases of irregular, rapid or slow beats then a 60 second count should be utilised.
Record the pulse rate on the patient record, including details about the rhythm and strength.
When taking a carotid pulse, the patient should lie down to reduce the risk of reflex bradycardia as this may cause reduction in blood pressure resulting in syncope.
Interpreting Results
Rate
Pulse rate refers to the number of times the hear beats per minute (bpm) and is a component in assessing the patient’s cardiovascular health.
Generally, a normal adult resting heart rate is between 60-100bpm. Below 60bpm is referred to as bradycardic and above 100bpm as tachycardic. However, these values are arbitrary and should be taken in context of the clinical situation.
The pulse rate is used to calculate the cardiac output, which is the volume of blood ejected by each ventricle per minute.
Cardiac Output = Heart Rate x Stroke Volume.
Hence, from the above equation, the heart rate is a factor that affects the cardiac output.
The pulse rate in a health patient tends to be relatively constant. However, in disease state of injury to the heart, the stroke volume is affected negatively (reduced), especially in cardiac muscle disease and reduced blood volume. In this case, to maintain the cardiac output, the heart rate needs to increase.
Causes of bradycardia
- Second degree heart block
- Third degree heart block
- Medication (beta blockers, digoxin)
- Sleep
- Hypothyroidism
- Athletes
Causes of tachycardia
- Pain
- Anxiety/Excitement
- Fever
- Medication (Vasodilators)
- Exercise
- Hyperthyroidism
- Cardiac arrhythmias (AF, SVT)
Rhythm
Pulse rhythm refers to the regularity or irregularity of the intervals between heartbeats. In healthy individuals, the pulse is typically regular and consistent. This regular pattern indicates the coordinated and efficient functioning of the heart’s electrical system.
Irregular pulse rhythms can occur it patients with underlying cardiovascular conditions. The irregularity in pulse rhythm is due to loss of co-ordination of the electrical conduction system (either rapid or delayed electrical discharge).
Causes of irregular pulses
- Sinus arrhythmia
- Atrial fibrillation
- Ventricular extrasystoles
- Atrial extrasystoles
- Second degree heart block
Rhythm identification
Regular
Regular intervals between heartbeats.
Irregularly irregular
Random pattern of pulsation. Normally associated with atrial fibrillation.
Regularly irregular
Irregular beat that occurs in a regular pattern, commonly seen in second degree hart blocks and pulsus bigeminies.
Regular with ectopic
Normal heart rate interrupted by an extra beat that causes the sequence to become out making the pulse feel irregularly irregular. ECG is needed to confirm this.
Strength/Character
Pulse strength or character refers to the quality and characteristics of the force of ejection of blood from the ventricles and the elasticity of the arterial wall. Different terms can be used to describe the pulse strength – weak, thready, strong, bounding, and full.
Weak/thready pulse
This can be a sign of reduced stroke volume secondary to disease or peripheral vascular disease. Causes of weak pulse can include bleeding, shock, heart failure, or dehydration.
Strong/bounding pulse
This may be felt during the times of high cardiac output or decreased peripheral resistance. Conditions such as exercise, heat, fever, anaemia, and other certain heart conditions.
Symmetry
Pulse symmetry refers to the equality or similarity of the pulses on both sides of the body. It involves comparing the rate, rhythm, and strength of the pulse inn corresponding pulse points.
This is not often routinely required unless clinical suspicion of conditions such as acute aortic dissection or obstruction of the arterial tree.
Pulses can also be felt simultaneously on the same side, such as the radial and femoral artery, and if there is a delay, this may also indicate an underlying condition.
Key Points
- The pulse is the rhythmic expansion and contraction of arteries caused by the heartbeat.
- It serves as a vital sign and provides information about heart rate, rhythm, and strength.
- Monitoring the pulse is crucial in assessing cardiovascular health and guiding medical interventions.
- Normal resting pulse rate for adults typically ranges between 60 and 100 beats per minute (bpm).
- Factors like age, fitness level, activity level, and underlying health conditions can influence the pulse rate.
Bibliography
British Heart Foundation (2015). What is a normal pulse rate? [online] BHF. Available at: https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/ask-the-experts/pulse-rate#:~:text=Your%20pulse%20rate%2C%20also%20known
Gregory, P. and Mursell, I. (2010). Manual of clinical paramedic procedures. Chichester: Wiley-Blackwell.