Prehospital Pulse Oximetry
Introduction
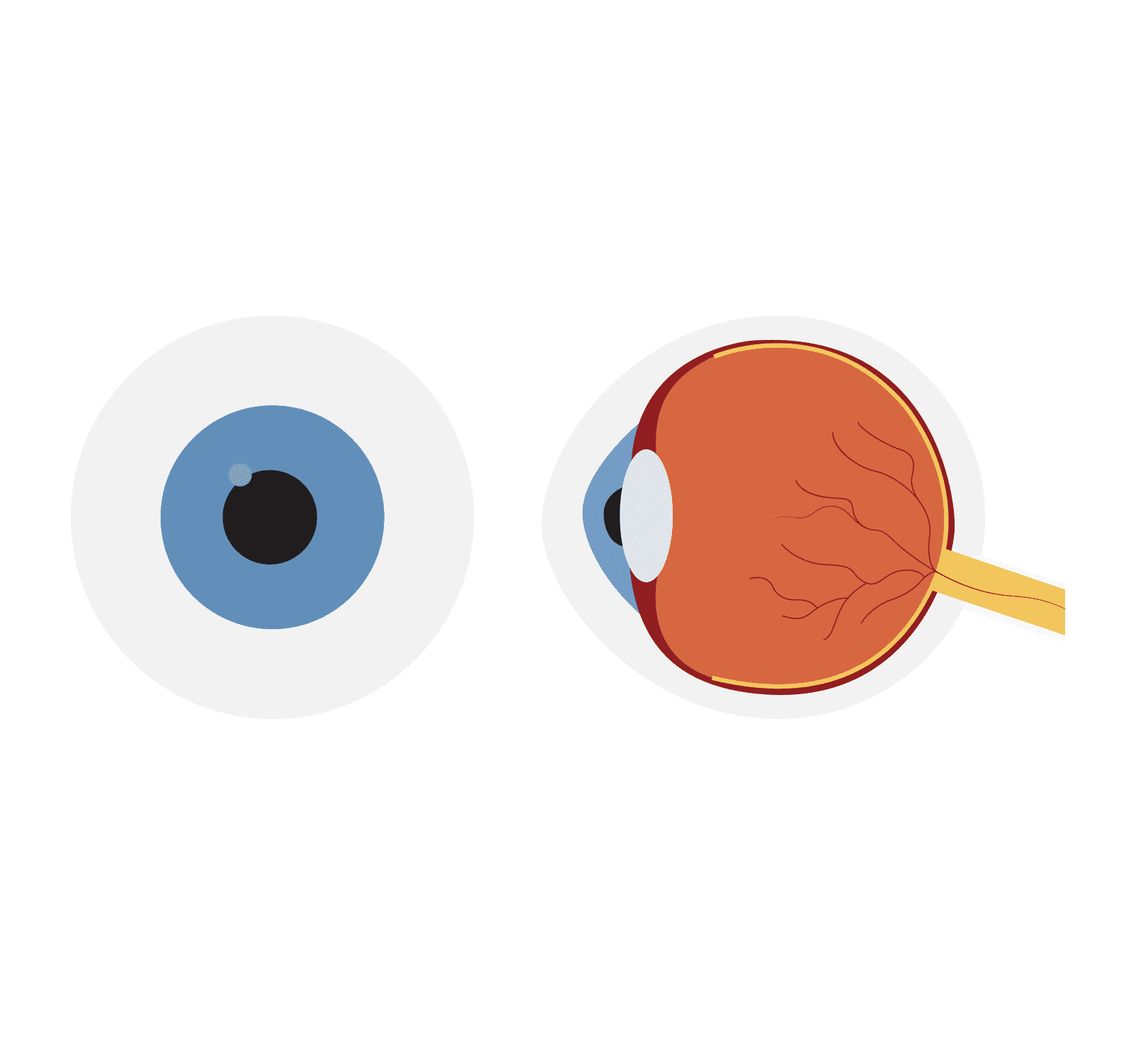
Prehospital pulse oximetry is a non-invasive way to measure the oxygen saturation in the blood. It is a valuable tool for emergency medical services (EMS) providers, as it can help them quickly assess a patient’s respiratory status.
Pulse oximetry is a non-invasive procedure used to measure the oxygen saturation level in a person’s blood. It provides valuable information about the efficiency of oxygen transport within the body. This technology is based on the principle that oxygenated blood absorbs and reflects light differently than deoxygenated blood.
Prehospital Pulse oximetry is widely used in various healthcare settings to assess respiratory health, evaluate the effectiveness of oxygen therapy, and detect early signs of hypoxia or respiratory distress.
PREHOSPITAL PULSE OXIMETRY INDICATIONS
Undertaking a prehospital pulse oximetry can help:
- Access respiratory function
- Review the efficacy of respiratory interventions.
- Gain baseline oxygen saturations prior to medical intervention.
Contraindications
None.
Cautions
While pulse oximetry is a valuable tool, it does have limitations that should be considered when performing prehospital pulse oximetry.
Poor Peripheral Circulation
Poor peripheral circulation affects pulse oximetry because it reduces the strength of the detected signals and impairs the delivery of oxygenated blood to the capillaries, leading to less accurate readings of oxygen saturation. Conditions such as cold or hypotension can result in these inadequate readings.
Carbon Monoxide Poisoning
Pulse oximeters measure the absorption of light by haemoglobin, and they cannot differentiate between oxygenated and carboxyhaemoglobin (COHb). In the presence of carbon monoxide, which binds to haemoglobin more strongly than oxygen, the readings may appear falsely high, leading to a potentially misleading assessment of oxygen saturation.
Motion
As pulse oximetry relies upon a steady pulse signal, excessive motion of digits from tremors, shivering, or seizures can interfere with signal detection.
Nail Polish
The presence of dark or opaque nail polish can obstruct the transmission of light through the nail bed, making it difficult for the pulse oximeter to accurately measure the absorption of light by the haemoglobin. This interference can lead to inaccurate readings of oxygen saturation levels.
Complications
None
PROCEDURE OF PREHOSPITAL PULSE OXIMETRY
Carry out pre-proecdure checks.
Ensure patient is relaxed and warm if possible.
Select a site for the probe, usually a finger or toes. Avoid shaking and cold extremities and nail varnish may need to be removed to aid accuracy.
Turn on the pulse oximeter, ensure it registers the pulse.
It is recommended that five minutes is given to allow the oximeter reading to settle prior to taking the reading.
When taking the reading, consider external factors and any limitations mentioned previously.
Factors Affecting Uptake Of Oxygen
Several factors can affect the uptake of oxygen in the body. These factors include:
Lung Function
There is much debate around the use and interpretation of capillary refill time, but as a quick and easy test that can be conducted in all haemodynamic status, it is likely to remain as part of a cardiovascular observation tool.
Respiratory Rate
A person’s respiratory rate, or the number of breaths per minute, plays a role in oxygen uptake. If the respiratory rate is too slow or too fast, it can impact the amount of oxygen taken in and carbon dioxide expelled.
Cardiac Output
The heart’s ability to pump oxygenated blood to the body’s tissues is crucial for oxygen uptake. Conditions that affect cardiac output, such as heart failure or certain heart diseases, can limit the delivery of oxygen to the tissues.
Haemoglobin Levels
Haemoglobin is the protein in red blood cells that carries oxygen. If the haemoglobin levels are low, as in cases of anaemia or bleeding, the oxygen-carrying capacity of the blood is reduced, affecting overall oxygen uptake.
Exercise
During physical activity, oxygen demand increases to meet the body’s metabolic needs. Factors such as intensity and duration of exercise, as well as overall metabolic rate, can influence oxygen uptake.
Altitude
At higher altitudes, the air pressure and oxygen levels are lower. This can lead to decreased oxygen uptake, especially for individuals not acclimated to the altitude.
Interpreting Results
Monitoring oxygen saturations help clinicians to decide if medical interventions are needed, such as administering oxygen.
The steepness of the oxyhaemoglobin dissociation curve, seen below, emphasizes the significance of even minor decreases in SpO2.

These reductions carry significant physiological and clinical implications, highlighting the crucial role of oxygen in aerobic cellular metabolism. The body’s compensatory mechanisms work to maintain a target of 100% oxygen saturation level, underscoring the importance of monitoring and addressing any deviations from optimal oxygen levels.
In individuals who were previously physically fit with normal respiratory and circulatory functions, a decrease in SpO2 of approximately ≥4% from the baseline should signal the necessity for a thorough evaluation of the patient’s other vital signs, including heart and respiratory rate. This assessment is crucial in determining the effectiveness of their compensatory mechanisms in response to the lowered SpO2 levels.
A decline in SpO2 of 8-10% indicates a considerable degree of hypoxemia, demanding an immediate and comprehensive clinical assessment to identify the underlying cause.
Oxygen Saturation (SpO2) Range:
Normal Range: In a healthy individual, a normal SpO2 level is typically above 96%.
Mild Hypoxemia: SpO2 levels between 91% and 94% may indicate mild oxygen desaturation.
Moderate Hypoxemia: SpO2 levels between 86% and 90% suggest moderate oxygen desaturation and potential respiratory impairment.
Severe Hypoxemia: SpO2 levels below 85% indicate severe oxygen desaturation and require immediate medical attention.
COPD Range: Normal SpO2 levels in patients with COPD are typically between 88% and 92%.
It’s important to remember that pulse oximetry readings provide a snapshot of oxygen saturation and pulse rate at a given moment. They should be interpreted in conjunction with the patient’s clinical condition, symptoms, and medical history. Other factors such as respiratory rate, blood pressure, and overall clinical assessment should also be considered to make a comprehensive evaluation of the patient’s oxygenation status. If there are concerns or significant deviations from normal, it is advisable to consult a healthcare professional for further evaluation and appropriate management.
Key Points
- Prehospital Pulse oximetry is a non-invasive medical technique used to measure the oxygen saturation level in a person’s blood.
- Oxygen saturation (SpO2) is expressed as a percentage and represents the proportion of haemoglobin molecules carrying oxygen compared to the total haemoglobin capacity in the blood.
- Certain factors can affect the accuracy of pulse oximetry readings, such as low perfusion, movement artifacts, ambient light interference, the presence of dyes or pigments, and impaired circulation.
- Pulse oximetry has limitations, including potential inaccuracies in specific clinical conditions, interference from carbon monoxide, and its inability to provide information about partial pressure of oxygen (PaO2) or carbon dioxide (PaCO2) levels.
- Normal ranges of SpO2 are above 96% in health patients and between 89% and 92% in patients with COPD.
References
Gregory, P. and Mursell, I. (2010). Manual of clinical paramedic procedures. Chichester: Wiley-Blackwell.
Torp, K.D., Modi, P. and Simon, L.V. (2023). Pulse Oximetry. [online] PubMed. Available at: https://www.ncbi.nlm.nih.gov/books/NBK470348/#:~:text=Pulse%20oximetry%20is%20a%20non
Wells (2009). Oxygen-Hemoglobin Dissociation Curve – an overview. [online] Science Direct. Available at: https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/oxygen-hemoglobin-dissociation-curve
Introduction
Pulse oximetry is a non-invasive procedure used to measure the oxygen saturation level in a person’s blood. It provides valuable information about the efficiency of oxygen transport within the body. This technology is based on the principle that oxygenated blood absorbs and reflects light differently than deoxygenated blood.
Pulse oximetry is widely used in various healthcare settings to assess respiratory health, evaluate the effectiveness of oxygen therapy, and detect early signs of hypoxia or respiratory distress.
Indications
Undertaking a pulse oximetry can help:
- Access respiratory function
- Review the efficacy of respiratory interventions.
- Gain baseline oxygen saturations prior to medical intervention.
Contraindications
None.
Cautions
While pulse oximetry is a valuable tool, it does have limitations that should be considered when performing pulse oximetry.
Poor Peripheral Circulation
Poor peripheral circulation affects pulse oximetry because it reduces the strength of the detected signals and impairs the delivery of oxygenated blood to the capillaries, leading to less accurate readings of oxygen saturation. Conditions such as cold or hypotension can result in these inadequate readings.
Carbon Monoxide Poisoning
Pulse oximeters measure the absorption of light by haemoglobin, and they cannot differentiate between oxygenated and carboxyhaemoglobin (COHb). In the presence of carbon monoxide, which binds to haemoglobin more strongly than oxygen, the readings may appear falsely high, leading to a potentially misleading assessment of oxygen saturation.
Motion
As pulse oximetry relies upon a steady pulse signal, excessive motion of digits from tremors, shivering, or seizures can interfere with signal detection.
Nail Polish
The presence of dark or opaque nail polish can obstruct the transmission of light through the nail bed, making it difficult for the pulse oximeter to accurately measure the absorption of light by the haemoglobin. This interference can lead to inaccurate readings of oxygen saturation levels.
Complications
None
Procedure
Carry out pre-proecdure checks.
Ensure patient is relaxed and warm if possible.
Select a site for the probe, usually a finger or toes. Avoid shaking and cold extremities and nail varnish may need to be removed to aid accuracy.
Turn on the pulse oximeter, ensure it registers the pulse.
It is recommended that five minutes is given to allow the oximeter reading to settle prior to taking the reading.
When taking the reading, consider external factors and any limitations mentioned previously.
Factors Affecting Uptake Of Oxygen
Several factors can affect the uptake of oxygen in the body. These factors include:
Lung Function
There is much debate around the use and interpretation of capillary refill time, but as a quick and easy test that can be conducted in all haemodynamic status, it is likely to remain as part of a cardiovascular observation tool.
Respiratory Rate
A person’s respiratory rate, or the number of breaths per minute, plays a role in oxygen uptake. If the respiratory rate is too slow or too fast, it can impact the amount of oxygen taken in and carbon dioxide expelled.
Cardiac Output
The heart’s ability to pump oxygenated blood to the body’s tissues is crucial for oxygen uptake. Conditions that affect cardiac output, such as heart failure or certain heart diseases, can limit the delivery of oxygen to the tissues.
Haemoglobin Levels
Haemoglobin is the protein in red blood cells that carries oxygen. If the haemoglobin levels are low, as in cases of anaemia or bleeding, the oxygen-carrying capacity of the blood is reduced, affecting overall oxygen uptake.
Exercise
During physical activity, oxygen demand increases to meet the body’s metabolic needs. Factors such as intensity and duration of exercise, as well as overall metabolic rate, can influence oxygen uptake.
Altitude
At higher altitudes, the air pressure and oxygen levels are lower. This can lead to decreased oxygen uptake, especially for individuals not acclimated to the altitude.
Interpreting Results
Monitoring oxygen saturations help clinicians to decide if medical interventions are needed, such as administering oxygen.
The steepness of the oxyhaemoglobin dissociation curve, seen below, emphasizes the significance of even minor decreases in SpO2.

These reductions carry significant physiological and clinical implications, highlighting the crucial role of oxygen in aerobic cellular metabolism. The body’s compensatory mechanisms work to maintain a target of 100% oxygen saturation level, underscoring the importance of monitoring and addressing any deviations from optimal oxygen levels.
In individuals who were previously physically fit with normal respiratory and circulatory functions, a decrease in SpO2 of approximately ≥4% from the baseline should signal the necessity for a thorough evaluation of the patient’s other vital signs, including heart and respiratory rate. This assessment is crucial in determining the effectiveness of their compensatory mechanisms in response to the lowered SpO2 levels.
A decline in SpO2 of 8-10% indicates a considerable degree of hypoxemia, demanding an immediate and comprehensive clinical assessment to identify the underlying cause.
Oxygen Saturation (SpO2) Range:
Normal Range: In a healthy individual, a normal SpO2 level is typically above 96%.
Mild Hypoxemia: SpO2 levels between 91% and 94% may indicate mild oxygen desaturation.
Moderate Hypoxemia: SpO2 levels between 86% and 90% suggest moderate oxygen desaturation and potential respiratory impairment.
Severe Hypoxemia: SpO2 levels below 85% indicate severe oxygen desaturation and require immediate medical attention.
COPD Range: Normal SpO2 levels in patients with COPD are typically between 88% and 92%.
It’s important to remember that pulse oximetry readings provide a snapshot of oxygen saturation and pulse rate at a given moment. They should be interpreted in conjunction with the patient’s clinical condition, symptoms, and medical history. Other factors such as respiratory rate, blood pressure, and overall clinical assessment should also be considered to make a comprehensive evaluation of the patient’s oxygenation status. If there are concerns or significant deviations from normal, it is advisable to consult a healthcare professional for further evaluation and appropriate management.
Key Points
- Pulse oximetry is a non-invasive medical technique used to measure the oxygen saturation level in a person’s blood.
- Oxygen saturation (SpO2) is expressed as a percentage and represents the proportion of haemoglobin molecules carrying oxygen compared to the total haemoglobin capacity in the blood.
- Certain factors can affect the accuracy of pulse oximetry readings, such as low perfusion, movement artifacts, ambient light interference, the presence of dyes or pigments, and impaired circulation.
- Pulse oximetry has limitations, including potential inaccuracies in specific clinical conditions, interference from carbon monoxide, and its inability to provide information about partial pressure of oxygen (PaO2) or carbon dioxide (PaCO2) levels.
- Normal ranges of SpO2 are above 96% in health patients and between 89% and 92% in patients with COPD.
Bibliography
Gregory, P. and Mursell, I. (2010). Manual of clinical paramedic procedures. Chichester: Wiley-Blackwell.
Torp, K.D., Modi, P. and Simon, L.V. (2023). Pulse Oximetry. [online] PubMed. Available at: https://www.ncbi.nlm.nih.gov/books/NBK470348/#:~:text=Pulse%20oximetry%20is%20a%20non
Wells (2009). Oxygen-Hemoglobin Dissociation Curve – an overview. [online] Science Direct. Available at: https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/oxygen-hemoglobin-dissociation-curve